Links to various Aetna Better Health and non-Aetna Better Health sites are provided for your convenience. Aetna Better Health is not responsible or liable for non-Aetna Better Health content accuracy or privacy practices of linked sites or for products or services described on these sites.
Essential care during trying times: You may be eligible for Medicaid during and after the COVID-19 crisis.
 By Eric Spitznagel
By Eric Spitznagel
TITLE: Lots of people have questions right now.
SEARCH BAR: Affordable slow-cooker recipes?
SERACH BAR: Good prices on cat food?
SERACH BAR: Best hair clippers?
SERACH BAR: Math homework help?
TITLE: Some questions are harder to ask.
GONZALO: What if I keep my job but I get furloughed?
ISAIAS: What if I lose my health insurance?
TITLE: You’re not alone.
TITLE: Millions of people have lost their health insurance in 2020.
TITLE: Many of them are now on Medicaid.
HANNA: What if I’m pregnant? What if it’s twins?
FAY: What about my kids? Can they be covered?
TITLE: Children can be covered by Medicaid, too.
ISAIAS: My kids are covered, but what if my nephew moves in?
FAY: What if I’m responsible for my disabled brother?
TITLE: Other family members may be eligible for Medicaid even if you aren't.
TITLE: Find out if you or your family qualifies for Medicaid.
GONZALO: Where do I start?
TITLE: Visit AetnaBetterHealth.com and choose your state.
LOGO: Aetna Better Health
Member names and other details have been omitted or fictionalized to protect the members’ identity
Paula A. remembers driving home from her office in mid-April with a pit in her stomach. Along with dozens of her coworkers, she’d just been laid off from her job in Illinois where she’d worked for almost a decade. The reason was the coronavirus.
“It was like having the rug pulled out from under me,” says this mother of multiple children who is in her 40s. “I always assumed this was where I’d work till I retired. My security, my family’s security, was tied up in this job.” Paula was the family’s sole breadwinner. They had savings, but not enough to last forever. There were mortgages to be paid and college tuitions on the horizon.
One immediate worry was health insurance. Paula relied on her employer for insurance. She had the option of buying into her longtime insurance plan, “but the costs were too much,” she says. “It just wasn’t something we could afford.”
Paula is far from alone. Over 40 million people have lost their jobs since the COVID-19 pandemic took hold in this country back in March.
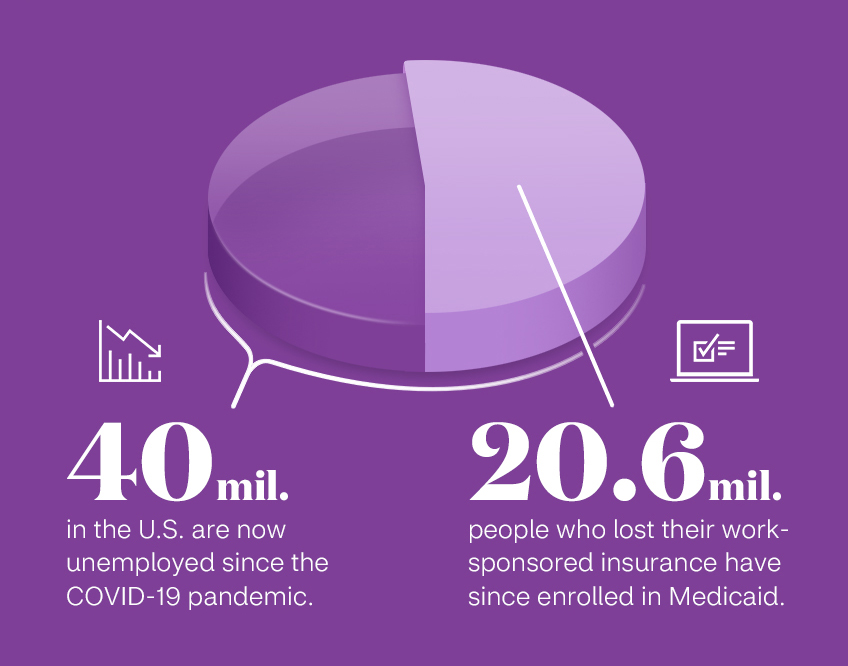
40 mil. in the U.S. are now unemployed since the COVID-19 pandemic. 20.6 mil. people who lost their work-sponsored insurance have since enrolled in Medicaid.
She considered applying for Medicaid, the federal-and-state-funded health insurance program, but Medicaid eligibility seemed scary and uncertain to her. “Did I even qualify for Medicaid?” she asks. “What are the financial requirements? I had no idea. So much of it was a mystery to me.”
But as Paula learned, finances can change for anyone, often suddenly and unexpectedly. Finding solutions in places you never expected is a sign of strength, not weakness. You may even discover that a temporary setback might end up putting you and your family on a more stable path to better health.
Almost half of American adults have postponed or skipped medical care due to the coronavirus outbreak.1 Paula fell into that group. “When I lost my job and my insurance, I canceled my annual checkup,” says Paula.
Paula realized she was neglecting more than just her own health. Her child has a nut allergy, and their medicine was close to expiring. “We could take our chances and hope for the best,” Paula says. "What if the worst happened? And it was all because I was too proud? I couldn’t live with myself.” A Medicaid plan with Aetna was the right answer — the only answer — for Paula and her family.
Medicaid is there even when the worst happens. Just days before the shelter-in-place order was issued in California in March 2020, Christopher B. was diagnosed with the coronavirus.
It was just the latest in ongoing health issues for this student in his late 20s who lives in California. He’s had chronic health conditions for years, and due to a change in his circumstances, he made the decision to transition to Medi-Cal, California's Medicaid program. Applying for it was easy — “a social worker at the hospital did it all for me,” Christopher says. “I just had to sign a couple of forms.” But his biggest fear was losing his regular team of doctors.
“I was forced to switch care teams,” he says. “That really upset me. The doctors who first started taking care of me since my diagnosis didn’t take Medi-Cal, so I had to switch to another hospital.”
But it was a blessing in disguise. “It was honestly the best thing that’s ever happened to me,” Christopher insists. “My new team is incredible. I feel like I’m getting the best care of my life. And it’s all because of Medicaid. At the time, it felt like a concession. I had to sign up for it because I couldn't afford anything else, and I didn’t have a choice. But honestly, this is exactly where I need to be.”
When he developed symptoms of COVID-19, his care team got him tested on the same day he came into the office and set him up with the necessary care. “I’ve never felt so taken care of in my life,” he says of his doctors. And then he adds with a laugh, “I’ve also never received a bill. That’s something to feel good about right there.”
Paula soon discovered the same thing about the ease of applying for Medicaid. “It was easier than I thought,” she says. “I was expecting a lot of hoops and paperwork, but it wasn’t complicated at all.”
The process is fairly simple: visit the Aetna Better Health site in your state and click on the “Become a member” section. You can also contact your state Medicaid agency or fill out an application through the Health Insurance Marketplace. This government screener can also help you determine if you qualify.

For both Paula and Christopher, signing up for Medicaid was one of the best decisions they made for their health. Paula was impressed with some of the extra benefits she and her family received by becoming Medicaid members with Aetna Better Health.
“We’ve all been dealing with a lot of stress because of the coronavirus,” she says. “But this takes some of that stress away.” She’s had her annual checkup through telemedicine, and her child has the peanut allergy medicine they need. It was all fully covered. “It’s hard to describe the feeling,” Paula says. “There are still struggles, but now I know our health isn’t one of them.”
1 https://www.forbes.com/sites/brucejapsen/2020/05/27/poll-nearly-half-of-us-adults-skipping-care-amid-pandemic/#3006e96e2273
About the author
Eric Spitznagel is a frequent contributor to Vanity Fair, Billboard, Men's Health, Playboy, The New York Post, and the New York Times Magazine, among others. He's published eight books, including his latest "Old Records Never Die: One Man's Quest for His Vinyl and His Past." He lives in Chicago with his wife and an 8-year-old amateur scientist.
Not yet a member?
See if Aetna Better Health® Medicaid coverage is available in your state.


